Apex Recovery, situated in the vibrant city of Nashville, TN, focuses on providing expert care for individuals grappling with substance abuse and alcohol dependency. Specializing in comprehensive rehabilitation and mental health treatment, Apex Recovery is dedicated to guiding individuals toward lasting recovery and holistic well-being.
At Apex Recovery, we understand the importance of accessible treatment options. We gladly accept various health insurance plans to facilitate the recovery process for our clients. Moreover, Apex Recovery may be a viable option for those considering rehabilitation treatment and who are covered by Humana insurance. We encourage you to contact our knowledgeable and compassionate team to determine your insurance coverage for your specific rehab needs.


Who Is Humana?
Established in 1961, Humana has emerged as a pivotal player in American healthcare, prioritizing enhancing individual and community well-being. Humana’s success is based on its commitment to comprehensive health care solutions.
Humana offers a range of products, from individual health coverage to group plans, tailored to address its extensive customer base’s varied and evolving needs. Humana has also made significant strides in Medicare, crafting innovative and customized plans to meet the escalating demand for reliable coverage among seniors, contributing to the company’s impact on the broader healthcare landscape. Beyond insurance offerings, Humana has demonstrated a commitment to holistic health through wellness programs that empower individuals to take charge of their health.
Some of Humana Brands and Services in Nashville, TN
In the dynamic healthcare landscape surrounding Nashville, Tennessee, Humana is a leading provider with a diverse portfolio of brands and services, offering a comprehensive approach to individual and community well-being.
- Humana Health Plans: Humana provides an extensive range of health insurance plans, ensuring coverage for a spectrum of medical services, from routine check-ups to specialized treatments. Their health plans often include wellness programs and preventive care initiatives, promoting a proactive approach to health.
- Humana Dental Plans: With a focus on holistic health, Humana’s dental plans go beyond basic coverage. They offer a suite of services, including routine cleanings, dental exams, and coverage for various dental procedures, fostering oral health for members in the Nashville area.
- Humana Vision Plans: Recognizing the importance of eye care, Humana’s vision plans encompass a wide array of services, from comprehensive eye exams to coverage for prescription eyewear. This ensures that members have access to essential vision care to maintain optimal eye health.
- Humana Medicare Plans: Tailored to the needs of seniors, Humana’s Medicare plans provide robust coverage, including hospital stays, doctor visits, and prescription medications. These plans are designed to address the unique healthcare requirements of individuals in the Nashville community who are navigating their golden years.
- Humana Pharmacy: Emphasizing convenience and accessibility, Humana Pharmacy services streamline the prescription fulfillment process. Members near Nashville can benefit from home delivery options, ensuring they have easy access to necessary medications for their health and well-being.
- Humana Behavioral Health Services: Humana recognizes the integral role mental health plays in overall well-being. Their behavioral health services encompass a range of support, including counseling and therapy, contributing to a holistic approach to healthcare.
- Humana at Home Services: Focused on enabling aging individuals to age in place, Humana at Home services provide various in-home care options, including caregiver support, tele-health services, and assistance with daily living activities.
Our insurance page goes further into depth with services and compares insurance plans for your convenience
What Is Humana Rehab Coverage?
Humana rehab coverage pertains to the array of rehabilitation services catered specifically for individuals dealing with substance abuse or addiction issues. This coverage extends to various therapeutic interventions aimed at aiding individuals in overcoming dependencies on alcohol, drugs, or other substances.
So, does Humana cover rehab? Yes, typically, Humana covers addiction rehab care and keeps a holistic approach to treatment in mind. Covered services typically include medical detoxification, counseling, behavioral therapy, and support groups, all of which are integral components of comprehensive addiction treatment.
Humana’s addiction rehab coverage encompasses both inpatient care and outpatient care, offering flexibility to policyholders based on the intensity of care required. Inpatient rehab may involve stays in specialized addiction treatment centers for immersive and closely monitored care, while outpatient services allow individuals to receive support and treatment while continuing to live in their communities. The goal of addiction rehab coverage is to help patients on their journey to recovery. Coverage aims to foster sobriety, improve mental health, and encourage relapse prevention.

Do Humana Insurance Policies Cover Substance Addiction Rehab in Nashville, TN?
Yes, Humana Insurance policies may cover addiction rehab, but the amount of coverage depends on the specific healthcare plan. Coverage for Humana alcohol rehab and Humana drug rehab may include detoxification, inpatient and outpatient treatment, and therapy. It’s crucial to check your policy details, including copayments and deductibles, to understand the specifics of addiction rehab coverage under your plan.
Does Humana Cover Medical Detox in Nashville?
Yes, Humana generally provides coverage for medical detox as part of its health insurance plans. However, you should check the specifics of your healthcare plan to confirm the extent of medical detox coverage and better understand what you may pay out of pocket for treatment.
Medical detox for addiction involves a supervised and medically managed process of helping individuals safely withdraw from substances such as drugs or alcohol. It’s conducted in a controlled environment, often a specialized facility, where medical professionals can monitor and manage withdrawal symptoms. Medications may be given to help alleviate discomfort and ensure a safer transition to sobriety. The goal is to address the physical aspects of addiction withdrawal while preparing individuals for ongoing treatment, recovery, and sobriety.
Does Humana Cover Residential Rehab in Nashville, TN?
Yes, Humana generally offers coverage for residential rehab as part of its health insurance plans. However, it is advisable to review your policy details to verify the extent of residential rehab coverage and gain a clearer understanding of potential out-of-pocket expenses for your treatment.
Residential rehab is an intensive treatment option where individuals struggling with addiction live on-site for a more extended period, typically from a couple of weeks to a few months. It offers:
- 24/7 supervision
- a structured schedule with therapeutic interventions such as individual and group therapy
- detoxification if needed
- a focus on education and skill-building
The environment fosters peer support and takes a holistic approach, addressing the physical, mental, and emotional aspects of addiction. Residential rehab programs also include aftercare planning to support individuals as they transition back to daily life, emphasizing the prevention of relapse through ongoing therapy and support groups. This format provides a focused and supportive setting for those with severe addiction issues, allowing them to dedicate themselves to recovery away from everyday triggers and distractions.
Does Humana Cover Dual Diagnosis Treatment in Tennessee?
Yes, Humana typically covers dual diagnosis treatment, which addresses mental health and substance abuse issues at the same time. Coverage details vary based on individual plans, so it’s essential to consult Humana directly or review policy documents for specific information regarding the extent of coverage for dual diagnosis treatment and related services.
Get a Free Assessment
Ask us to check your insurance coverage.
Other Rehab Treatment Programs Covered by Humana in Nashville, TN
Apex Recovery offers a range of rehab treatment programs near Nashville, TN, all covered by Humana. With Humana’s support, individuals can access Apex’s partial hospitalization programs (PHP), intensive outpatient programs (IOP), and inpatient rehab for those needing a higher level of support.
Humana Coverage for Partial Hospitalization Programs
Partial hospitalization programs (PHP) for addiction rehab offer a balanced approach, providing intensive treatment while allowing individuals to return home each day. These programs, typically structured with therapy sessions and support, cater to those who need a higher level of care than outpatient services but don’t require 24/7 treatment. PHPs contribute to a comprehensive and effective addiction recovery journey.
Humana in Nashville typically covers the costs associated with partial hospitalization programs, making these crucial services more accessible to those seeking addiction recovery.
Humana Coverage for Intensive Outpatient Program
The intensive outpatient program (IOP) in addiction rehab provides a flexible yet comprehensive approach, offering therapy and support without the need for full-time residency. Designed for patients requiring more care than standard outpatient services, IOP allows participants to maintain daily life commitments while benefiting from intensive treatment. This balanced approach fosters effective addiction recovery within a supportive and accommodating framework.
In Nashville, Humana typically covers the costs associated with intensive outpatient programs (IOP) for addiction recovery. This coverage enhances accessibility to crucial services, ensuring individuals receive structured therapy and support without full-time residency. Humana’s commitment to covering IOP expenses facilitates a comprehensive and flexible approach, empowering individuals in their journey toward effective addiction recovery within a supportive framework.
Humana Coverage for Inpatient Rehab
Inpatient rehab programs for addiction provide 24/7 structured care within a therapeutic environment. Offering intensive support and supervision, these programs are designed for individuals requiring a highly immersive approach to addiction recovery. With a focus on comprehensive treatment, inpatient rehab programs contribute to breaking the cycle of addiction, promoting healing, and providing a foundation for long-term recovery.
Humana typically covers the costs associated with inpatient rehab programs for addiction, enhancing accessibility to vital services for those on the path to recovery. This coverage ensures individuals receive 24/7 structured care within a therapeutic environment, promoting comprehensive healing and recovery. Humana’s commitment to covering inpatient rehab program expenses underscores its support for individuals seeking intensive and immersive treatment for addiction.
Rehab Center Near Nashville, TN That Takes Humana
In the continuous effort to combat addiction, individuals pursuing recovery frequently seek assistance from specialized treatment centers. For those covered by Humana, identifying appropriate rehab centers that take Humana is a pivotal phase in their path to well-being.
With a commitment to comprehensive care and evidence-based interventions, Apex Recovery, a Humana-approved treatment center, assumes a crucial role in addressing the distinctive requirements of patients who struggle with alcoholism or drug addiction. At Apex Recovery, we welcome various insurance policies, including Humana, to facilitate the journey toward recovery.
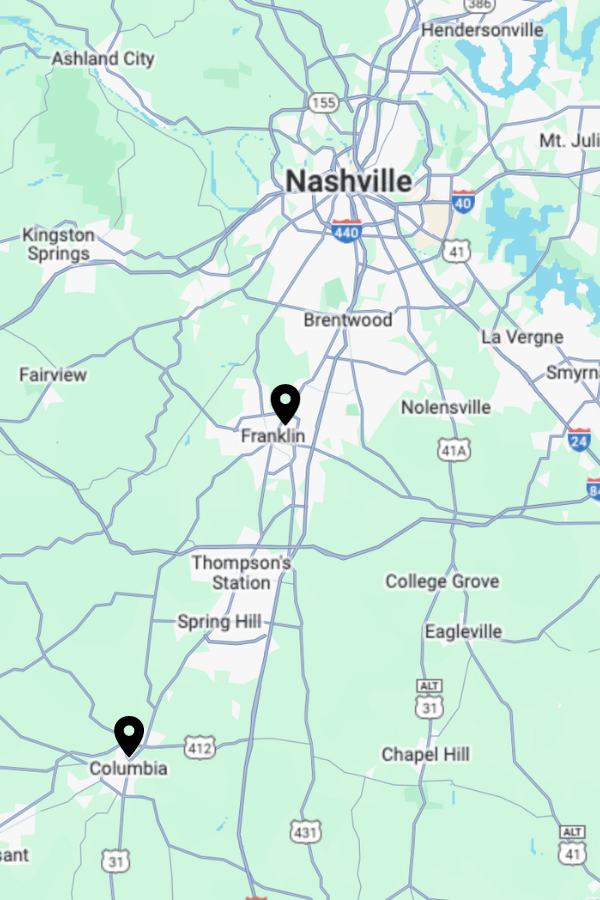
Apex Recovery Franklin
4601 Carothers Pkwy STE 250A
Franklin, TN 37067
Apex Recovery Columbia
2710 Trotwood Ave STE A & B
Columbia, TN 38401
Discovering Nashville, Tennessee and Its Vibrant Towns
Situated in the heart of Tennessee, Nashville stands out not only for its rich musical legacy but also as a hub for a variety of industries and institutions. This city, with its iconic country music scene, dynamic neighborhoods, and thriving artistic culture, flaunts a unique mix of southern charm and modern vitality. Nashville’s location on the Cumberland River provides a scenic backdrop that enhances its allure.
Moving outwards from the city, Williamson County rises as a noteworthy region. Renowned for its suburban tranquility, historic sites, and high-quality schools, it exudes a distinct character. Whether you seek the city’s energetic rhythm or the county’s serene ambience, the area delivers diverse experiences.
Right at the top, Davidson County, home to Nashville’s urban core, sprawls over a considerable metropolitan expanse. Famed for its music landmarks, cultural attractions, and diverse communities, Davidson County is a metropolitan hub that captures the essence of Tennessee’s urban verve.
Each of these areas contributes to the unique mosaic of Nashville, and their close proximity allows locals and visitors to enjoy the varied landscapes and opportunities this region offers.
Drug and Alcohol Addiction Statistics in Nashville
In Nashville, Tennessee, the city grapples with substantial challenges brought on by drug and alcohol addiction. The statistics reflect a considerable problem that contributes to a serious public health crisis. A sizeable number of Nashville’s population battles with addiction to various substances such as opioids, methamphetamines, and alcohol.
The accessibility of illicit drugs in Nashville, in addition to social and cultural influences, has led to an increased prevalence of addiction. A 2022 report, titled Substance Use in Tennessee: Prevalence and Treatment, indicates 48% of residents aged 12 and over have consumed alcohol in the last 30 days, while 18% admitted to marijuana use in the past year. In the same period, 8% of Tennesseans met the criteria for a Substance Use Disorder (SUD).
From 2018 to 2020, there was a close to 40% increase in emergency department visits related to non-heroin opioid use. During the same period, the number of establishments offering residential care and hospital inpatient care for substance use treatment saw a 60% increase.
Only about 35% of health plan members under commercial HMO and PPO plans diagnosed with alcohol or other drug dependence received care adhering to the national quality standard, with an initial treatment visit within 14 days of diagnosis.
Sources:
- https://www.samhsa.gov/
- https://www.tn.gov/health.html
- Please complete and send the form below.
- One of our staff members will contact your insurer to check your coverage.
- We will contact you promptly with the results and to discuss the next steps.
Insurance Verification
"*" indicates required fields
What Is the Average Cost of Addiction Rehab in Nashville With Humana Insurance?
The average cost of addiction rehab in Nashville with Humana insurance varies depending on factors such as the specific treatment program, duration, and individual policy details. Generally, Humana insurance coverage can significantly offset expenses for medical detox, therapy, and other addiction rehabilitation services.
The average cost of addiction rehab in Nashville with insurance varies widely. Prospective patients should check on their Humana insurance policy for accurate information on coverage and potential out-of-pocket expenses.
How To Check Humana Coverage Levels for Rehab Treatment in Nashville, TN
To assess Humana coverage for rehab treatment, contact their customer service or log in to their website. Review the policy documents or speak with a representative to understand coverage levels, including inpatient or outpatient rehab services, therapy sessions, and medication.
You can also contact us at Apex Recovery to verify network provider coverage and inquire about any pre-authorization requirements to ensure a smooth and covered rehabilitation process. Stay informed to maximize benefits and minimize out-of-pocket expenses.
How To Get Humana To Pay For Rehab Treatment in TN
Getting Humana to pay for rehab treatment involves navigating a process that includes verifying coverage, obtaining prior authorization if required, and ensuring that the treatment meets the insurer’s criteria. Here are steps to ensure Humana pays for your rehab treatment.
- Verify Insurance Coverage: Contact Humana to verify your insurance coverage for rehab treatment. Ask about the specifics of your rehab insurance coverage, including whether rehab treatment is covered, what types of treatment are included, and any limitations or restrictions.
- Understand Your Plan: Familiarize yourself with your insurance plan documents and seek details on mental health and substance abuse treatment coverage.
- In-Network Providers: Check if the rehab facility you’re considering is in-network with Humana. In-network providers typically have pre-negotiated rates with the insurance company, which can reduce your out-of-pocket costs. If possible, choose an in-network facility, like Apex Recovery, to increase the likelihood of coverage.
- Pre-Authorization: Determine if pre-authorization, sometimes called pre-certification or prior authorization, is required for rehab treatment. This is a process where your healthcare provider obtains approval from Humana before you receive certain services. Apex Recovery can help you submit the necessary information and documentation to Humana for pre-authorization.
- Medical Necessity: Humana may require evidence of medical necessity for rehab treatment. This could include a comprehensive assessment from a qualified healthcare professional like those at Apex Recovery.
- Appeal Process: If your initial request for coverage is denied, familiarize yourself with Humana’s appeal process. You have the right to appeal a denial. Apex Recovery will work closely with you to gather additional information that may support your case and submit a formal appeal to Humana.
- Patient Advocacy: Consider seeking assistance from a patient advocacy organization or a healthcare advocate who can guide you through the insurance process and help you navigate any challenges.
Remember that the process for ensuring Humana covers your treatment may vary depending on your specific plan. It’s essential to be proactive, communicate with your healthcare provider and insurance company, and be persistent in pursuing coverage for rehab treatment.
How Many Times Will Humana of Tennessee Pay For Rehab?
The number of times Humana of Tennessee will pay for addiction rehab may vary based on the individual’s insurance plan and the terms outlined in their policy. Insurance coverage for addiction rehab typically depends on factors such as the type of plan, the specific treatment needed, and whether the facility is in or out of the network.
It is crucial for patients seeking addiction treatment to contact Humana directly or review their insurance policy to understand better the addiction rehab coverage details, including how many times Humana will pay for rehab. At Apex Recovery, we can help you figure out the rehab admissions process, which includes helping you verify your Humana insurance coverage.