Apex Recovery, an addiction rehab treatment center located in Nashville, Tennessee, is dedicated to transforming lives through specialized drug and alcohol addiction rehab, as well as mental health treatment. Apex Recovery is committed to providing patients with the support they need to overcome their addiction and achieve lasting sobriety.
At Apex Recovery, we understand that seeking treatment is an important step towards a healthier life. We strive to make our comprehensive services accessible to those in need by accepting various health insurance plans. Potential coverage is available for individuals considering rehab treatment with UnitedHealthcare (UHC). To verify your insurance coverage for rehab, you should contact our team.


Who Is UnitedHealthcare?
UnitedHealthcare is a prominent health insurance provider founded in 1977. Offering a diverse range of health-related products and services, they specialize in health plans for individuals, employers, and government programs. UnitedHealthcare is renowned for its commitment to improving healthcare accessibility and quality, serving millions of customers nationwide.
The company’s comprehensive offerings include medical, dental, vision, and prescription drug coverage and innovative wellness and care management programs. UnitedHealthcare typically offers coverage for addiction rehab treatment as part of its behavioral health services. The specific coverage and available treatment options may vary depending on the plan and location. Generally, UnitedHealthcare plans include services such as inpatient and outpatient treatment for substance use disorders, detoxification programs, counseling, therapy, and support groups.
Some of UHC Brands and Services Near Nashville
UnitedHealthcare operates various brands and services in Tennessee. Here are some of their key offerings in Tennessee:
- UnitedHealthcare Insurance Company: This is the main insurance entity that provides many different types of health insurance plans, including family plans, individual plans, employer-sponsored plans, and government-sponsored plans.
- UnitedHealthOne: This brand may be associated with individual and family health insurance plans.
- UnitedHealthcare Community Plan: This is often associated with Medicaid and other government-sponsored health programs, providing coverage for eligible individuals and families.
- Optum: While Optum is a separate business segment under the UnitedHealth Group umbrella, it plays a crucial role in healthcare services and management. It includes OptumRx for pharmacy benefits management and Optum Health for health and wellness services.
- UnitedHealthcare Employer & Individual: This division provides health insurance coverage for employers and individuals, offering a range of plans and benefit options.
- UnitedHealthcare Medicare & Retirement: This segment focuses on Medicare Supplement Insurance plans, Medicare Advantage plans, and other products tailored to the needs of Medicare beneficiaries.

What Is UHC Rehab Coverage?
UHC Addiction Rehab Coverage refers to the addiction rehabilitation coverage provided by UnitedHealthcare (UHC), one of the largest health insurance providers in the country. This coverage typically includes various addiction treatment services such as detoxification, inpatient care, outpatient care, and counseling for individuals struggling with alcoholism or substance abuse.
So, does UHC cover rehab? Yes, UnitedHealthcare covers alcohol rehab and drug rehab. Through that coverage, UHC aims to support its members in overcoming addiction by offering comprehensive coverage for evidence-based treatments and therapeutic interventions.
Does UnitedHealthcare Cover Substance Addiction Rehab in TN?
Yes, UnitedHealthcare typically provides coverage for substance addiction rehab. The amount of coverage may vary depending on the specific plan, so reviewing the policy details is crucial. Generally, UnitedHealthcare drug rehab plans include benefits for inpatient and outpatient treatment services, encompassing detoxification, counseling, and other necessary therapies.
Individuals seeking rehab services should contact UnitedHealthcare to verify their specific coverage and explore available treatment options, or contact us at Apex Recovery, and we can help you verify your UHC insurance coverage.
Does UnitedHealthcare Cover Medical Detox?
UnitedHealthcare may cover medical detox services as part of its health insurance plans. However, coverage can vary depending on plan details. Medical detox typically involves supervised withdrawal from substances under medical care to manage withdrawal symptoms and ensure a safer process.
Medical detox, or detoxification, is a supervised process aimed at helping individuals safely withdraw from substances like drugs or alcohol. Conducted under the care of medical professionals in specialized facilities, the goal is to manage withdrawal symptoms and ensure the individual’s safety. This includes the following:
- Close monitoring of vital signs,
- Medical interventions to alleviate discomfort and, in some cases,
- Administration of medications
Medical detox serves as the first step in addiction treatment, preparing individuals for ongoing rehabilitation. However, it is not a standalone solution; comprehensive addiction treatment programs, including therapy and support groups, are usually necessary to address underlying issues and foster long-term recovery.
Does UHC Cover Residential Rehab?
UHC (UnitedHealthcare) typically covers residential rehab services as part of its comprehensive health insurance plans. Residential rehab, often utilized for the treatment of substance abuse or mental health disorders, involves round-the-clock care in a specialized facility. UHC’s coverage for residential rehab may vary depending on the specific plan, with considerations for medical necessity and pre-authorization.
You should review your policy details to understand better the extent of residential rehab coverage and any potential out-of-pocket costs associated with residential rehab services.
Does UHC Cover Dual Diagnosis Treatment in TN?
Yes, UHC (UnitedHealthcare) typically covers dual diagnosis treatment. Dual diagnosis means individuals are facing both mental health and substance use disorders at the same time. UHC aims to provide comprehensive dual-diagnosis healthcare. Treatment for dual diagnosis often includes therapy, medication, and support services.
Dual diagnosis treatment is a specialized approach aimed at addressing the simultaneous presence of a mental health disorder and a substance use disorder. This comprehensive strategy integrates psychotherapy, such as cognitive-behavioral and dialectical behavior therapies, along with medication management to stabilize mood and manage symptoms. Support services, including group therapy and support groups, play a key role in creating a supportive community for recovery. The integrated care approach recognizes the interconnected nature of mental health and substance use, emphasizing the need to address both conditions concurrently for effective and lasting recovery.
Get a Free Assessment
Ask us to check your insurance coverage.
Other Rehab Treatment Programs Covered by UnitedHealthcare Near Nashville
Apex Recovery offers a diverse range of addiction rehabilitation treatment programs in Nashville, and most are typically covered by UnitedHealthcare insurance plans. Through UnitedHealthcare, individuals can access treatment options such as partial hospitalization programs (PHP), intensive outpatient programs (IOP), and inpatient rehab.
UHC Coverage for Partial Hospitalization Programs
Partial hospitalization programs (PHP) are intensive, structured outpatient mental health programs designed to provide comprehensive treatment for individuals dealing with mental health issues. These programs offer more care than outpatient services, allowing participants to return home in the evenings.
A PHP involves a range of therapeutic interventions, including individual and group therapy, medication management, and skill-building activities, aimed at addressing the specific needs of individuals struggling with psychiatric disorders or emotional challenges. The goal is to prevent or reduce the need for inpatient hospitalization and encourage relapse prevention by providing a supportive and therapeutic environment during the day.
UnitedHealthcare (UHC) typically covers partial hospitalization programs as part of its mental health coverage. UHC is a leading health insurance provider offering a range of plans, and mental health coverage is often included. Coverage for PHPs may vary depending on the specific plan and policy details, so individuals should review their policy documents or contact UHC directly to learn more about Partial Hospitalization Programs.
UHC Coverage for Intensive Outpatient Program
An intensive outpatient program (IOP) is a type of addiction rehab treatment that offers a higher level of care than outpatient therapy. It is for individuals who require more support than standard outpatient services but do not need a partial hospitalization or inpatient program. IOPs typically involve individual therapy, support groups, and medication management.
These programs provide individuals with the flexibility to keep their daily routines while still getting the necessary therapeutic interventions to address and manage their mental health challenges. UnitedHealthcare (UHC) generally covers intensive outpatient programs as part of its mental health coverage. UHC is committed to providing comprehensive mental health services to its members, recognizing the importance of accessible and effective treatment options. However, coverage specifics may vary based on the individual’s insurance plan and policy details.
UHC Coverage for Inpatient Rehab
Inpatient rehabilitation programs provide a higher level of care for individuals dealing with various alcohol or substance abuse issues. These programs typically involve a residential setting where individuals stay for a specified period, receiving round-the-clock medical supervision, intensive therapy, and comprehensive support.
In the context of substance abuse, inpatient rehab programs often focus on detoxification, counseling, and skill-building to help patients with addiction to develop the tools needed for sustained recovery. For medical conditions, inpatient rehabilitation may involve therapies and interventions to regain physical or cognitive function following surgery, illness, or injury.
UnitedHealthcare (UHC) generally covers inpatient rehabilitation as part of its health insurance offerings. UHC is a major health insurance provider that understands the importance of comprehensive care for individuals facing medical challenges or substance abuse issues. However, inpatient rehab coverage can vary based on the insurance plan and policy details.
Rehab Center Near Tennessee That Takes UnitedHealthcare
Individuals seeking addiction recovery treatment often seek support from specialized rehabilitation centers near Nashville. Finding appropriate rehab facilities that accept UnitedHealthcare coverage for those covered by UHC is a vital milestone in the sobriety journey. Qualified addiction rehab centers are committed to delivering thorough care and evidence-based interventions to help patients recover from addiction.
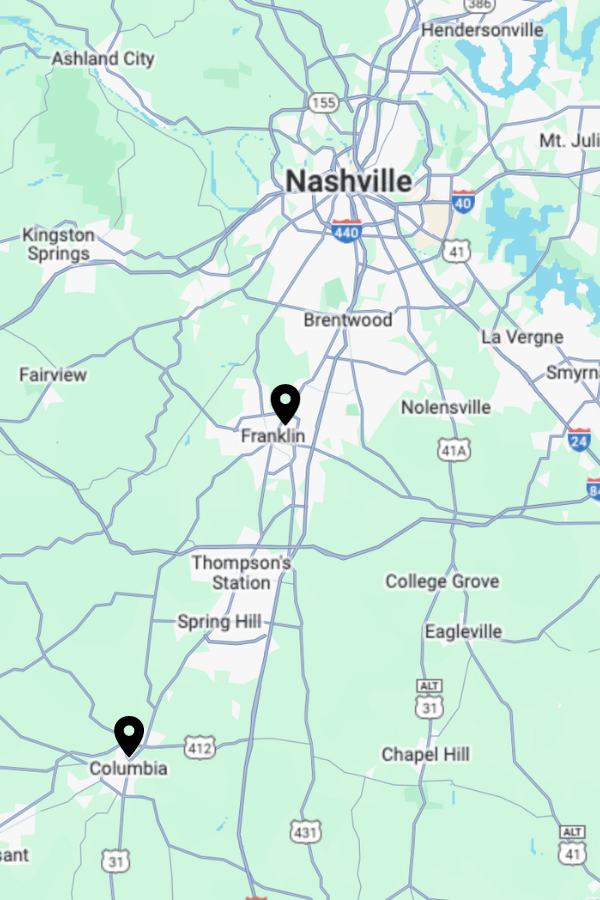
Apex Recovery operates two treatment centers in Tennessee. We extend our assistance to patients grappling with alcoholism or drug addiction, and we accept a range of insurance plans, including UHC, to help individuals on their journey to recovery.
Apex Recovery Franklin:
4601 Carothers Pkwy STE 250A Franklin, TN 37067
Apex Recovery Columbia:
2710 Trotwood Ave STE A & B Columbia, TN 38401
- Please complete and send the form below.
- One of our staff members will contact your insurer to check your coverage.
- We will contact you promptly with the results and to discuss the next steps.
Insurance Verification
"*" indicates required fields
What Is the Average Cost of Addiction Rehab in Tennessee With UHC Insurance?
While the average cost of addiction rehab around Nashville with UnitedHealthcare (UHC) insurance fluctuates depending on several factors, such as the treatment center’s location and amenities, the specifics of the insurance coverage play a crucial role. UnitedHealthcare typically offers a range of plans, each with its level of coverage for addiction treatment services, which may include:
- Detoxification
- Inpatient or outpatient therapy
- Counseling sessions
- Follow-up care
It’s important to note that some UHC plans might have network restrictions, which may offer better coverage for rehab facilities within their network. Therefore, individuals considering addiction rehab in Nashville should verify that their chosen facility is within the UHC network to maximize insurance benefits.
Additionally, the duration of the rehabilitation program can impact costs, with longer-term treatments often incurring higher expenses. Ultimately, obtaining a clear understanding of both the insurance policy and the rehab facility’s fees is essential for individuals seeking addiction treatment to make informed decisions about their recovery journey.
How To Check UHC Coverage Levels for Rehab Treatment
To check your UnitedHealthcare (UHC) rehab treatment coverage, contact customer service or log in to the UnitedHealthcare website. Reviewing your insurance policy to understand coverage levels for inpatient or outpatient rehab services, therapy sessions, and medication is important.
You may contact us at Apex Recovery to verify your provider coverage and inquire about pre-authorization requirements. Staying informed is essential to maximize your insurance benefits and minimize out-of-pocket expenses.
If you require rehab treatment and are uncertain about what your insurance covers, you can contact us online or call (877) 881-2689 for assistance.
How To Get UnitedHealthcare To Pay For Rehab Treatment
Getting UnitedHealthcare (UHC) to cover rehab treatment involves navigating a process that includes verifying coverage, obtaining prior authorization if required, and ensuring that the treatment meets the insurer’s criteria. To facilitate the process of getting UHC to cover rehab treatment, it’s crucial to start by reviewing your policy to understand available coverage for addiction rehabilitation services better.
You can check UHC’s online resources to gather information on specific requirements and procedures or contact us at Apex Recovery for help. If prior authorization is necessary, you can start the approval process to avoid delays in accessing behavioral health treatment. Additionally, collaborate closely with your healthcare providers to align the proposed rehab program with UHC’s criteria, ensuring that the chosen treatment plan aligns with the insurer’s guidelines. By staying proactive and informed throughout these steps, you can increase the likelihood of a successful approval process, enabling UHC to cover the necessary rehab treatment.
How Many Times Will UnitedHealthcare Pay For Rehab in Nashville?
How many times UnitedHealthcare (UHC) covers addiction rehab expenses may vary depending on the individual’s insurance plan and the terms outlined in their policy. Coverage for addiction rehab under UHC insurance is generally influenced by factors such as the type of plan, the specific treatment required, and whether the facility is within the network.
It is imperative for individuals seeking addiction treatment to contact UHC directly or review their insurance policy to gain a comprehensive understanding of the addiction rehab coverage details, including the number of times UHC will pay for rehab. At Apex Recovery, we are ready to assist you in navigating the rehab admissions process and offer support in verifying your insurance coverage.

Exploring Nashville, Tennessee and its Notable Features
Tennessee is often celebrated for its rich history, dynamic culture, and the iconic City of Nashville. Nashville, a crown jewel of Tennessee, distinguishes itself with its engaging music scene, lively downtown, and rich civil war history.
Situated in the central part of the state, Nashville enjoys a moderate subtropical climate, making it a welcoming destination throughout the year. Visitors can explore the historic Broadway district, unwind in Centennial Park, or marvel at the splendor of the Cumberland River’s tranquil shores. Nashville is also home to the thriving hub of Music Row. Known as the heart of Nashville’s entertainment industry, Music Row is a convergence of musical talent, home to record labels, radio stations, and the legendary RCA Studio B. Its varied neighborhoods offer a blend of style and charm, from the upscale boutiques of The Gulch to the historic appeal of East Nashville.
Drug and Alcohol Addiction Statistics in Nashville and Tennessee
- 4,330,771 Opiod Painkiller Subscriptions were given to residents of Tennessee
- In 2021, there were 3,814 fatalities due to drug overdoses in Tennessee
- In the Nashville-Davidson-Murfreesboro-Franklin MSA, 9.3 percent of people age 12 or older were classified as with a substance use disorder. This is higher than the Tennessee average which sat at 8 percent over the same time period
- One study shows that in 2020 about 77% of all fatal drug overdoses had traces of fentanyl in the toxicology report