Apex Recovery is a leading rehabilitation center with locations in San Diego and Tennessee that specializes in comprehensive treatment for drug and alcohol addiction as well as mental health issues. Accepting various health insurance plans, we strive to ease the financial burden for individuals seeking recovery.
Veterans may also find support through Apex Recovery, as the facility may accept Veterans’ insurance. If you or a loved one are seeking treatment for substance abuse, contact us at Apex Recovery to explore your insurance coverage details and discuss tailored treatment options, ensuring a smoother path to healing.

Free Addiction Assessment
Schedule a free, confidential assessment with a licensed clinician. Apex Recovery can check your insurance coverage levels for drug and alcohol addiction, and mental health treatment.
What is Veterans Insurance?
Veterans Insurance is an overarching term used to describe the healthcare coverage and benefits provided to individuals who have served in the United States military. The Department of Veterans Affairs (VA) is the federal agency responsible for administering these benefits. Veterans insurance primarily encompasses a wide range of health services, including hospital care, mental health services, prescription medications, and more.
One notable aspect of veterans’ healthcare is the VA Community Care Network, facilitated by third-party administrators (TPAs) like TriWest. The VA Community Care program allows eligible veterans to access healthcare services from private providers when VA facilities may be distant or unable to provide timely care. TPAs are crucial in coordinating and managing this community care network, ensuring veterans receive quality healthcare services promptly. The nation strives to honor its commitment to the health and well-being of those who have served in the military through the combination of the VA, veterans insurance, and community care programs.
Who is TriWest?
TriWest is a third-party administrator who collaborates closely with the VA to facilitate the Community Care Network (CCN) administration. As a key partner in delivering healthcare services to eligible veterans, TriWest plays a pivotal role in ensuring access to quality medical care through the CCN when VA facilities may be geographically distant or have capacity constraints.
The collaboration between TriWest and the VA is instrumental in ensuring that veterans receive timely, quality healthcare through the CCN. TriWest manages logistics for the Community Care program, connecting veterans with private healthcare providers. This partnership enhances the accessibility of medical services for veterans, efficiently and effectively addressing their diverse healthcare needs. Through its commitment to supporting the well-being of those who have served in the military, TriWest is a key facilitator in the broader framework of veterans’ healthcare.
What is Veteran Addiction Rehab Treatment Coverage?
Veteran addiction treatment coverage refers to the extent of healthcare benefits and financial assistance provided to veterans for addressing substance abuse issues. The Department of Veterans Affairs (VA) offers this coverage, which may encompass various services such as counseling, rehabilitation programs, and medications tailored to support veterans in their journey to sobriety.
The goal is to ensure that veterans have access to comprehensive and specialized care to overcome substance abuse challenges, emphasizing their overall well-being and successful reintegration into civilian life.
- Please complete and send the form below.
- One of our staff members will contact your insurer to check your coverage.
- We will contact you promptly with the results and to discuss the next steps.
Insurance Verification
"*" indicates required fields

Rehab Center in San Diego, CA That Treats Veterans
Apex Recovery provides a Veteran’s treatment program unique from other Veteran addiction treatment centers. Our integrated and holistic approach combines addiction recovery with trauma recovery and addresses dual diagnosis simultaneously through evidence-based methods like cognitive-behavioral therapy (CBT) and motivational interviewing.
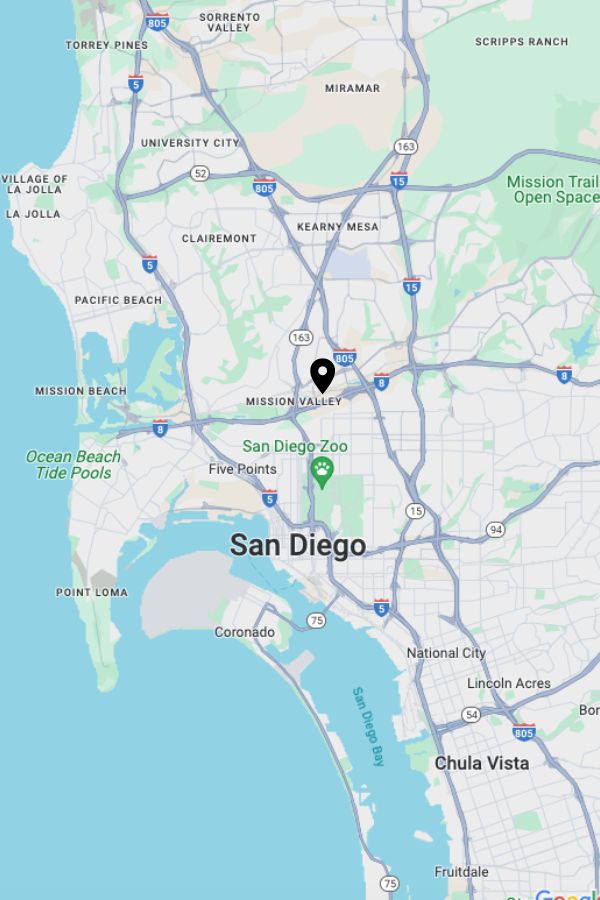
With relapse prevention in mind, our rehabilitation program delivers comprehensive care and support to meet the distinct needs of veterans seeking recovery. We accept insurance and are looking forward to discussing your treatment needs. Call (877) 881-2689or visit our San Diego-based treatment facility today:
Apex Recovery San Diego: 2810 Camino del Rio S #106 San Diego, CA 92108
Free Addiction Assessment
Schedule a free, confidential assessment with a licensed clinician. Apex Recovery can check your insurance coverage levels for drug and alcohol addiction, and mental health treatment.
Does VA Insurance Cover Drug and Alcohol Treatment in CA?
VA insurance does cover drug and alcohol treatment. The extent of coverage varies based on the specific plan. The VA recognizes the importance of addressing substance abuse issues and provides financial assistance for treatment services. While the coverage levels may differ, veterans can expect at least some of the costs associated with drug and alcohol treatment to be covered.
Through the Community Care Network (CCN), veterans also have the option to receive treatment outside the traditional VA network. This flexibility allows veterans to access specialized care and rehabilitation services from private providers, expanding the range of available treatment options. By participating in the CCN, veterans can receive tailored, timely care for substance addiction issues, contributing to their overall well-being and recovery journey. Check your insurance coverage levels for drug and alcohol treatment now.
Does TriWest Cover Rehab in Southern California?
TriWest is a third-party administrator that manages certain aspects of the Department of Veterans Affairs (VA) healthcare programs, including the Community Care Network (CCN). TriWest collaborates with the VA to facilitate care for veterans when it’s not feasible for them to receive treatment at a VA facility. Through the CCN, TriWest may cover rehabilitation services for eligible veterans.
The specific coverage, eligibility criteria, and types of rehab services covered can vary based on individual circumstances and the terms of your health care plan. For accurate information about TriWest alcohol rehab and TriWest drug rehab coverage, contact TriWest directly or call (877) 881-2689. You can inquire about your eligibility, coverage levels, and the specific rehab services available through TriWest-administered programs.
Does Veterans Insurance Cover Medical Detox Programs?
Veterans Insurance typically covers at least some of the costs associated with medical detoxification programs, though the specific coverage levels vary based on the insurance plan. The Department of Veterans Affairs (VA) recognizes the importance of addressing substance abuse, including the need for medical detoxification, and provides financial support to veterans seeking such services.
Medical detoxification programs play a critical role in helping individuals safely withdraw from substances and manage withdrawal symptoms under medical supervision. Veterans can often utilize their insurance coverage to access these essential services, supporting them in the initial stages of their recovery journey. To get precise information about coverage levels and eligibility for medical detox, call (877) 881-2689.
Does Veterans Insurance Cover Residential Addiction Rehab in CA?
Veterans Insurance covers some of the costs for residential addiction rehab, but coverage levels vary based on the individual’s insurance plan. The Department of Veterans Affairs recognizes the importance of comprehensive treatment and financially supports veterans seeking residential rehabilitation. For specific details on coverage and eligibility, veterans should contact the VA or call (877) 881-2689.

Free Addiction Assessment
Schedule a free, confidential assessment with a licensed clinician. Apex Recovery can check your insurance coverage levels for drug and alcohol addiction, and mental health treatment.
Does Veterans Insurance Cover Mental Health Treatment?
Veterans Insurance generally covers at least some of the costs associated with mental health treatment. The Department of Veterans Affairs (VA) recognizes the significance of addressing mental health concerns and provides financial support for veterans seeking such services. However, the extent of coverage varies based on your insurance plan’s specific terms and conditions.
Mental health treatment may include therapy, counseling, and psychiatric services aimed at supporting veterans in managing and overcoming mental health challenges. Veterans can utilize their insurance coverage to offset some of the expenses. To obtain detailed information about coverage levels, eligibility, and specific mental health treatment options covered, contact us for personalized assistance.
Does Veterans Insurance Cover EMDR Therapy?
Yes, Veterans Insurance typically covers at least some of the costs associated with Eye Movement Desensitization and Reprocessing (EMDR) therapy. Recognizing the importance of evidence-based therapeutic approaches, the VA provides financial support for veterans seeking medically necessary EMDR therapy as part of their mental health treatment. The extent of coverage depends on the specific terms and conditions outlined in your plan.
EMDR therapy is a specialized form of psychotherapy effective in treating trauma and post-traumatic stress disorder (PTSD). Veterans can often use their insurance coverage to help offset expenses related to EMDR sessions, making this therapeutic option more accessible. Don’t hesitate to call Apex Recovery at (877) 881-2689 for personalized support in navigating your mental health treatment options. Our team is ready to provide detailed information on coverage levels and eligibility and connect you with experienced EMDR therapy providers. Your well-being is our priority, and we’re here to assist you in navigating your insurance coverage and recovery journey.
How To Check My Triwest Coverage Levels in California for Rehab Treatment
Apex Recovery is in-network with many insurance companies, making it easy to check your insurance coverage. Complete our no-obligation, confidential online form linked below, and our team will verify your insurance details. Specifically, for those utilizing TriWest for rehab treatment coverage, we’ll have a highly skilled staff member contact TriWest to confirm your insurance details.
Following this, we’ll reach out to you to review your policy and guide you in the following steps of the process. Moreover, if you’re dedicated and ready to begin your recovery journey, you can initiate the process by sending a request to one of our experienced rehab admissions coordinators today.
Our coordinators are prepared to address any inquiries or uncertainties you may have regarding Apex Recovery’s programs, offering detailed insights into pricing and the array of payment options available. Your dedication to recovery is of utmost importance to us, and we are committed to supporting you every step of the way. Feel assured that we are here to assist and guide you every step of the way.

Other Rehab Treatment Programs Covered by Veterans Insurance in California
Veterans Insurance often extends support to various other rehabilitation treatment programs. The Department of Veterans Affairs (VA) is committed to ensuring that veterans receive comprehensive, tailored care to address multiple health concerns. Below, we highlight specific areas of rehabilitation typically covered by Veterans Insurance. It’s essential to note that the extent of coverage can vary based on your particular plan.
Veterans Insurance Coverage for Partial Hospitalization Programs
A partial hospitalization provides intensive outpatient treatment for mental health and substance abuse issues, offering structured therapy during the day with the flexibility for individuals to return home in the evenings. Notably, Veterans Insurance, including plans administered by TriWest, typically covers PHPs for eligible veterans.
This reflects the ongoing commitment of the Department of Veterans Affairs (VA) to ensuring comprehensive access to mental health and rehabilitation services. Check your insurance plan details or call (877) 881-2689 for specific PHP coverage and eligibility information.
Veterans Insurance Coverage for Intensive Outpatient Program
An intensive outpatient represent a higher level of structured treatment for individuals dealing with mental health or substance abuse issues. Outpatient care does not require 24-hour supervision and usually involves therapeutic activities such as group counseling, individual therapy, and educational sessions, providing a comprehensive, supportive environment while allowing for the maintenance of daily routines.
Veterans Insurance, including plans administered by TriWest, typically extends coverage for eligible veterans for IOPs—call (877) 881-2689 for specific coverage and eligibility information.
Veterans Insurance Coverage for Inpatient Rehab
Inpatient rehabilitation is a service often accommodated by Veterans Insurance, is a specialized approach to delivering round-the-clock care for severe mental health or substance abuse issues. Inpatient care involves individuals residing in a facility for an extended period, fostering an environment for intensive therapeutic interventions, medical monitoring, and supportive recovery surroundings.
Explore the coverage details of inpatient rehabilitation under Veterans Insurance, including plans managed by TriWest in collaboration with the Department of Veterans Affairs (VA). For personalized insights into your insurance plan specifics, coverage levels, and eligibility criteria for inpatient rehab, connect with us at (877) 881-2689. We’re here to provide detailed information to guide you through your recovery journey.
Veterans Insurance Coverage for Evidence-Based Therapy and Treatments
Veterans Insurance proactively supports evidence-based therapy and treatments, emphasizing scientifically proven approaches to meet the mental health and recovery needs of Veterans. This dedication is evident in TriWest-administered plans under the Department of Veterans Affairs (VA), guaranteeing eligible veterans access to therapies with proven effectiveness.
For personalized insights into coverage levels and eligibility criteria for evidence-based therapy and treatments, review your insurance plan details and contact us at Apex Recovery. We stand ready to provide specific information to ensure the quality care you or your loved one deserves.
How To Get TriWest to Pay for Addiction Rehab
To utilize TriWest coverage for addiction rehabilitation, follow these structured steps:
- Obtain Referral: For mental health or substance use disorder treatment through TriWest, you’ll need to obtain a referral from your primary care provider at the VA. This ensures that the services you receive are medically necessary and covered by your policy.
- Choose Treatment Provider: With a referral in hand, select rehab centers that take TriWest.
- Coordinate with Provider: After choosing a treatment provider, coordinate to ensure accurate billing of your TriWest policy. Provide your insurance information, including the policy number and relevant details so that the facility may submit claims on your behalf.
- Understand Cost-sharing Responsibilities: Depending on your plan, be aware of potential out-of-pocket expenses, such as copayments or deductibles. Comprehending your cost-sharing responsibilities before embarking on the treatment journey is crucial.
How Many Times Will TriWest Pay for My Treatment?
TriWest beneficiaries can generally obtain coverage for multiple rounds of rehab treatment, provided each round is deemed medically necessary and authorized by their healthcare provider. The extent of coverage may be subject to specific limitations, including a maximum number of days or a maximum dollar amount per year.
The frequency of TriWest’s coverage for rehab is contingent on various factors, such as the plan, the nature and duration of the required rehab treatment, and recommendations from the healthcare provider. TriWest’s managed care benefits operate within the framework of the VA Healthcare System, which may have its own regulations, exclusions, and limitations regarding the frequency of rehab treatment. For instance, the VA might mandate beneficiaries to undergo evaluation or secure additional medical clearance before authorizing multiple rounds of rehab treatment.
Addiction Statistics in California
- Information gleaned from the California Health Interview Survey (CHIS) spanning 2011–2013 indicated that around 90,000 veterans had mental health needs, with an additional 200,000 reporting serious thoughts of suicide within the 12 months before participating in CHIS.
- In addition to elevated rates of post-traumatic stress disorder (PTSD) and traumatic brain injury (TBI), the VA has identified that roughly 55% of homeless veterans grapple with mental health challenges. Substance abuse affects 70% of this population, and 40% of female homeless veterans report severe mental illness, often stemming from elevated instances of military sexual trauma.
- Governor Newsom suggested a plan for the 2024 ballot to enhance how California deals with mental illness, substance abuse, and homelessness. This includes a proposal that aims to provide housing for homeless veterans. The proposal also suggests updating the Mental Health Services Act to ensure a minimum of $1 billion annually for housing and care related to behavioral health.
- In 2018, the use of cannabis varied among veterans who were prescribed opioids, and the states with the highest cannabis use among these veterans were Oregon (25.2%), Washington (23.6%), and California (18.6%).
- Approximately 1 in 7 California veterans who own a firearm at home have contemplated suicide at some point.
- Of the veterans residing in homes with firearms, 18.0% indicated they required professional assistance for emotional, mental health, or substance use issues in the previous year.
- California teenagers exhibit a 24.46% higher likelihood of recent drug use compared to the average American teen.
- Fifty percent of Californians aged 12 and older acknowledged using alcohol in the last month, while 20% reported using marijuana in the past year.
- Approximately 2.7 million Californians qualified for a substance use disorder (SUD) in the previous year, yet only 10% sought any form of treatment.
- Six percent of Californians indicated they met the criteria for alcohol dependence, while 3% reported meeting the criteria for dependence on illicit drugs.
- The opioid prescription rate in California saw a 34% decline from 2010 to 2019.
