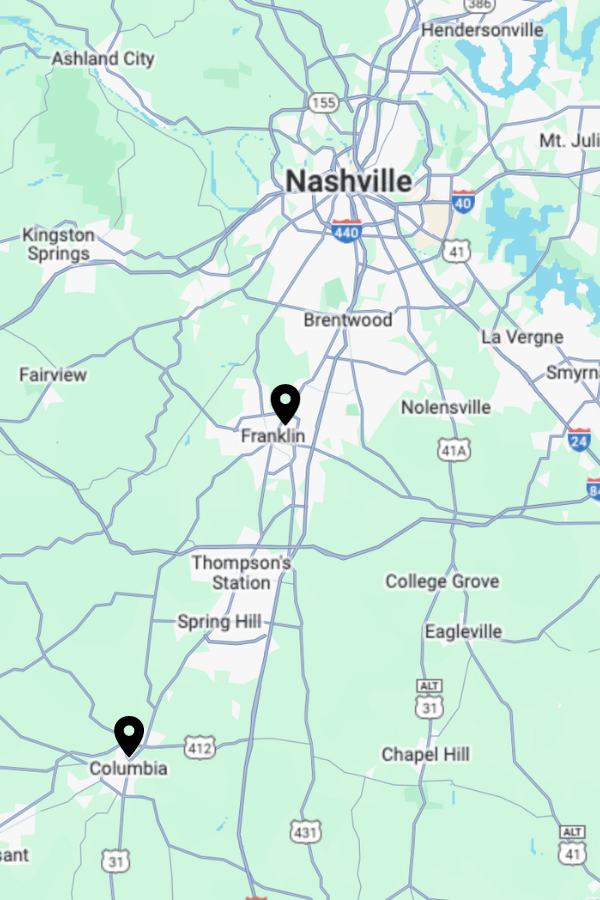
For those in Tennessee seeking effective drug and alcohol addiction rehab and mental health treatment, Apex Recovery, located just outside Nashville, is dedicated to providing compassionate care. With facilities like Apex Recovery Franklin (Outpatient) and Apex Recovery Columbia (Inpatient and Outpatient), we offer tailored programs for diverse needs.
We understand the financial concerns associated with rehabilitation, and that’s why we strive to make the process as transparent and accessible as possible. Apex Recovery accepts various health insurance plans for rehab treatment, including Aetna of TN. To learn more about your coverage levels and to verify if your Aetna insurance is accepted, reach out to our dedicated team. Contact Apex Recovery today, and let us assist you in taking the first step towards a healthier, substance-free life.

Exploring Nashville, TN and Cities Near Middle Tennessee
The region of Middle Tennessee boasts a diverse and picturesque landscape, offering residents and visitors alike a rich blend of urban amenities and natural beauty. Anchored by the vibrant city of Nashville, Middle Tennessee boasts cities that contribute to its unique charm. Franklin and Columbia, both home to Apex Recovery facilities, embody the region’s historic and cultural appeal.
As you explore further, you’ll encounter the bustling city of Murfreesboro, known for its thriving community and educational institutions, and Hendersonville, situated along the scenic shores of Old Hickory Lake. Middle Tennessee unfolds to include the enchanting town of Townsend, the lively city of Chattanooga, and the iconic destinations of Gatlinburg and Memphis. The region is also dotted with gems like Collierville and Oak Ridge, each offering a distinct flavor of Tennessee living. Whether you’re drawn to the music scene in Nashville, the historic allure of Germantown, or the natural wonders of Chattanooga, Middle Tennessee provides a diverse tapestry of experiences for those exploring its cities and landscapes.
Alcohol & Drug Addiction Statistics in Nashville, TN
In the Nashville metropolitan area, substance abuse poses a significant challenge, with 18.1% of residents reported to have used illicit drugs. Additionally, 6.4% of individuals in the Nashville area engaged in the misuse of prescription pain relievers. 9.3% of residents aged 12 and older experienced a Substance Use Disorder, reflecting a widespread issue spanning various age groups in the community.
The toll of substance abuse is starkly evident in the alarming number of suspected drug overdose deaths in 2021, exceeding 700. Of particular concern is the fact that 74% of these drug overdoses were related to fentanyl, indicating a heightened risk associated with potent opioids. The demographic distribution of these drug overdose deaths reveals that 67% of cases in Nashville were males. The economic burden of substance abuse in Tennessee is substantial, with an estimated cost of 2 billion dollars. Notably, approximately 70,000 Tennessee residents are estimated to be grappling with opioid addiction, highlighting the urgent need for comprehensive interventions and support services in the state.
Free Addiction Assessment
Schedule a free, confidential assessment with a licensed clinician. Apex Recovery can check your insurance coverage levels for drug and alcohol addiction, and mental health treatment.
Who is Aetna Insurance?

Aetna, a stalwart in the American health insurance landscape, boasts a rich history dating back to its founding in 1853. With a legacy of over a century and a half, Aetna has been a key player in the evolution of healthcare coverage. Recently, it reached a milestone when it was acquired by CVS Health, solidifying its position in the industry.
Aetna is renowned for providing a comprehensive suite of health insurance products and services. Their offerings span medical, dental, pharmacy, and behavioral health coverage, reflecting a commitment to addressing the diverse needs of individuals and families. Beyond insurance, Aetna has been a catalyst for initiatives aimed at enhancing overall well-being, demonstrating a dedication to shaping a healthier future for communities nationwide. As a vital contributor to the healthcare landscape, Aetna continues to play a crucial role in ensuring access to quality healthcare services for millions of Americans.
Some of Aetna Brands and Services in Tennessee
Aetna is dedicated to providing a spectrum of healthcare solutions in Tennessee. From comprehensive medical coverage to specialized services, Aetna’s diverse offerings cater to the unique needs of individuals in the state. Here’s an expanded list of some key Aetna brands and services available in Tennessee:
- Aetna Better Health of Tennessee: focuses on Medicaid and Medicare services, striving to improve access to quality healthcare for underserved populations in Tennessee. Their approach integrates medical, behavioral, and social services to enhance overall well-being.
- Aetna Dental: Aetna’s dental services extend across Tennessee, offering coverage for routine check-ups, preventive care, and more extensive dental procedures. Aetna Dental aims to support individuals in maintaining optimal oral health.
- Aetna Whole Health: these plans prioritize coordinated and integrated care, emphasizing collaboration among healthcare providers. In Tennessee, individuals enrolled in Aetna Whole Health plans benefit from a holistic approach that addresses their physical and mental health needs.
- Aetna Behavioral Health: Recognizing the significance of mental health, Aetna’s Behavioral Health services in Tennessee encompass a range of resources. This includes access to mental health professionals, counseling services, and programs designed to address various behavioral health challenges.
- Aetna Pharmacy: Aetna’s pharmacy services ensure that individuals in Tennessee have access to a wide range of prescription medications. Their network of pharmacies and prescription drug plans is designed to make essential medications more accessible and affordable.
- Aetna Vision: provides vision care coverage in Tennessee, offering benefits for eye exams, prescription glasses, and contact lenses. This service aims to promote eye health and enhance overall quality of life.
- Aetna Medicare Advantage Plans: provide seniors with comprehensive healthcare coverage. These plans often include additional benefits beyond traditional Medicare, such as vision, dental, and prescription drug coverage.
What is Aetna Rehab Coverage in Tennessee (TN)?
Aetna is a reliable source for comprehensive rehab coverage in Tennessee, addressing the critical needs of individuals contending with substance abuse. Their inclusive coverage spans both inpatient care and outpatient services, ensuring a continuum of care that includes essential components like detoxification, counseling, and immersive rehabilitation programs. Aetna supports recovery through a tailored approach to substance abuse treatment.
If you are seeking clarity on your rehab coverage in Tennessee, contact us at Apex today. Understanding the specifics of coverage not only facilitates informed decision-making but also empowers you to access the most suitable and effective treatment options. At Apex, we will help you understand the specifics of your Aetna policy and get you on your path to rehabilitation.
- Please complete and send the form below.
- One of our staff members will contact your insurer to check your coverage.
- We will contact you promptly with the results and to discuss the next steps.
Insurance Verification
"*" indicates required fields

Rehab Center in Tennessee That Takes Aetna
If you’re in Tennessee, seeking reputable rehab centers that take Aetna, look no further than Apex Recovery. As a leading facility dedicated to providing effective drug addiction and alcoholism rehab and mental health treatment, Apex Recovery understands the importance of accessible and comprehensive care. The good news is that Apex Recovery, with multiple locations in Middle Tennessee, accepts health insurance, including Aetna rehab coverage. Call us at 877.881.2689, contact us on our site, or stop by:
Apex Recovery Franklin
4601 Carothers Pkwy STE 250A
Franklin, TN 37067
Apex Recovery Columbia
2710 Trotwood Ave STE A & B
Columbia, TN 38401
Free Addiction Assessment
Schedule a free, confidential assessment with a licensed clinician. Apex Recovery can check your insurance coverage levels for drug and alcohol addiction, and mental health treatment.
Does Aetna Cover Substance Addiction Rehab in TN?
Aetna typically provides coverage for substance addiction rehab in Tennessee. Their comprehensive plans typically include support for both inpatient and outpatient rehabilitation services, ensuring individuals have access to essential treatments such as detoxification, counseling, and ongoing therapeutic programs. Aetna’s commitment to addressing substance addiction underscores their dedication to promoting holistic well-being and supporting individuals on their journey to recovery.
Understanding the specific details of Aetna’s coverage for substance addiction rehab in Tennessee is crucial for individuals seeking assistance. Contact Apex to explore the extent of your coverage, including any potential limitations or additional services offered. Our emphasis on transparency and personalized care contributes to a comprehensive and effective rehabilitation experience for those in need.
Does Aetna Insurance Cover Medical Detox in Tennessee (TN)?
Yes, Aetna insurance generally covers medical detox in Tennessee. Medical detoxification is a crucial step in overcoming substance addiction, and Aetna recognizes its significance by including it in their comprehensive coverage. This service is designed to provide individuals with a safe and supervised environment, ensuring proper medical support during the withdrawal process.
Medical detoxification is often a necessary initial phase in the treatment of substance addiction, allowing individuals to safely manage withdrawal symptoms under medical supervision. To gain a thorough understanding of the specific details of coverage, you are encouraged to review their policy documents and reach out to Apex for clarification. Call us today at 877.881.2689 or contact us online. You can also check your insurance any time to get started.
Does Aetna Cover Residential Rehab in Tennessee (TN)?
So, does Aetna cover rehab in Tennessee? Yes, it typically does cover residential rehab. Recognizing the importance of a supportive and immersive environment for addiction recovery, Aetna’s comprehensive coverage often extends to inpatient residential rehabilitation programs. These programs provide individuals with a structured and supervised setting, allowing for focused treatment, counseling, and support to foster lasting recovery.
Residential rehab is a critical component of substance addiction treatment, offering a highly structured and therapeutic environment that can be particularly beneficial for those with more severe addiction issues. To better understand the specifics of coverage and explore available residential rehab options, contact Apex Recovery directly for detailed information tailored to your needs. We can walk you through the rehab admissions process to put your mind at ease.

Average Cost of Addiction Rehab in Tennessee With Aetna Insurance?
Well, how much is rehab with Aetna insurance? The average cost of addiction rehab in Tennessee is influenced by factors like treatment type and program duration. Aetna’s coverage often results in a substantial reduction in out-of-pocket expenses for individuals seeking rehabilitation services. To gain clarity on specific coverage details and potential costs, reach out to the experts at Apex Recovery.
Apex’s dedicated team can provide personalized information regarding Aetna insurance coverage for addiction rehab, helping you make informed decisions about your treatment journey. Contacting Apex is a crucial step in navigating the financial aspects of rehabilitation and ensuring a smoother and more accessible path to recovery.
How To Check Aetna Coverage Levels for Rehab Treatment in TN
To check Aetna coverage levels for rehab treatment in Tennessee, reach out to Apex Recovery. The dedicated team at Apex is ready to assist and provide detailed information about Aetna insurance coverage, answering specific questions about rehab treatment options. Initiate this process by calling Apex directly or by visiting the online verification form at https://apex.rehab/verify-your-insurance/.
This user-friendly form allows you to input your insurance information, enabling Apex to assess coverage levels and guide you towards the most suitable and cost-effective treatment plan. Whether reaching out by phone or utilizing the online form, Apex’s commitment to transparency ensures that you receive the necessary information to make informed decisions about your recovery journey in Tennessee.
How To Get Aetna To Pay For Rehab Treatment in TN
To facilitate Aetna coverage for rehab treatment in Tennessee, you can take proactive steps to ensure a smoother process. Contact Apex, where the experienced team can guide you through the steps to get Aetna to pay for rehab treatment. We can assess coverage levels, answer questions, and assist in navigating the steps required to maximize Aetna’s support for rehab services.
By establishing direct communication with Apex, you can leverage the expertise of the facility’s staff in dealing with insurance providers. Our commitment to assisting individuals in obtaining Aetna coverage for rehab treatment ensures a more seamless and informed process, helping you focus on your recovery journey without unnecessary financial barriers.
How Many Times Will Aetna Insurance Pay For Rehab in Tennessee?
The frequency with which Aetna insurance will pay for rehab in Tennessee can vary based on individual policies and the specific details outlined in each plan. Aetna typically provides coverage for rehab services, but the number of times it will pay for rehab depends on factors such as the type of treatment, duration, and the specific terms of the policy.
To get precise information about the coverage limits and frequency of payment, individuals are encouraged to reach out to Apex Recovery directly. The experienced staff at Apex can assist in understanding the nuances of Aetna alcohol rehab in TN and guide individuals on how to optimize their coverage for Aetna drug rehab services.

Other Tennessee Rehab Treatment Programs Covered by Aetna
In addition to these treatments, Aetna insurance extends coverage to various other rehab programs in Tennessee, ensuring a broad spectrum of options to meet diverse needs. Aetna typically covers Partial Hospitalization Programs (PHP), offering individuals a structured yet flexible treatment approach that allows for intensive therapy during the day while providing the freedom to return home in the evenings.
Intensive Outpatient Programs (IOP) are also commonly covered, providing a step-down level of care for those who require ongoing support but do not need 24-hour supervision. For individuals requiring a more immersive and structured environment, Aetna’s coverage often includes Inpatient Rehab programs.
Aetna Insurance Coverage for Partial Hospitalization Programs (PHP)
Partial Hospitalization Programs (PHP) provide individuals with a structured and comprehensive form of outpatient care. Tailored for those who require intensive treatment but do not need 24-hour supervision, this level of care is ideal for those transitioning from more intensive inpatient treatment or for those who require focused support to manage their mental health or substance use challenges.
Aetna insurance typically covers Partial Hospitalization Programs (PHP), making this level of care more accessible for individuals in need. This coverage ensures that those enrolled in Aetna health plans in Tennessee can benefit from the structured and supportive environment offered by PHPs, facilitating their journey toward recovery.
Aetna Insurance Coverage for Intensive Outpatient Program (IOP)
The Intensive Outpatient Program (IOP) is a flexible and comprehensive outpatient treatment option, allowing participants to maintain their daily routines while receiving intensive therapy, counseling, and support. This level of care is beneficial for individuals transitioning from more intensive forms of treatment or for those requiring additional support as they navigate the challenges of mental health or substance use disorders.
Aetna insurance typically covers Intensive Outpatient Programs (IOP), making this level of care more accessible for individuals seeking comprehensive treatment in Tennessee. Contact us at Apex to understand the specifics of coverage for IOPs and the rehab admissions procedure, so you can make informed decisions about your treatment path.
Aetna Insurance Coverage for Inpatient Rehab
Inpatient Rehab is a comprehensive and highly structured form of treatment where individuals reside within a healthcare facility for an extended period. This level of care is designed for those with more severe mental health or substance use disorders, providing 24/7 supervision, intensive therapy, and a supportive environment conducive to recovery.
Aetna insurance typically covers Inpatient Rehab, providing individuals in Tennessee with access to comprehensive and immersive treatment options. This coverage ensures that individuals enrolled in Aetna health plans can receive the necessary care within a residential setting, where they can focus solely on their recovery journey. Call us today at (619)458-3435 to learn more.
Does Aetna Cover Dual Diagnosis Treatment in TN?
In general, Aetna insurance covers dual diagnosis treatment in Tennessee. Dual diagnosis programs aim to provide individuals with tailored interventions, addressing the interplay between mental health conditions and addiction. Aetna’s commitment to covering these specialized programs shows their dedication to holistic healthcare and supporting individuals in their journey toward lasting recovery.
The Affordable Care Act (ACA) has significantly contributed to the expansion of mental health and substance use disorder services across the nation. By designating these services as essential health benefits, the ACA ensures that individuals have improved access to integrated behavioral health services. The combined efforts of Aetna’s coverage and the ACA’s provisions create a more supportive environment for individuals seeking dual diagnosis treatment in Tennessee, emphasizing the importance of addressing both mental health and substance use in tandem for optimal outcomes.
Alcohol & Drug Addiction Statistics in Nashville, TN
- 18.1% of Nashville metropolitan area residents used illicit drugs
- 6.4% of Nashville-area residents misused prescription pain relievers
- 9.3% of those aged 12 years and older had a Substance Use Disorder
- Over 700 suspected drug overdose deaths in 2021
- 74% of drug overdoses in 2021 were fentanyl-related
- 67% of drug overdose deaths in Nashville were males
- 2 billion dollar cost to the state for substance abuse
- 70,000 estimated opioid-addicted Tennessee residents

